Scientists have been praising CAR-T cells (chimeric antigen receptor T cells) for its potential to treat leukaemia and lymphoma, two blood malignancies, for the past few years. These cells are designed to attach to malignant blood cells and eliminate particular marks, or antigens, on them.
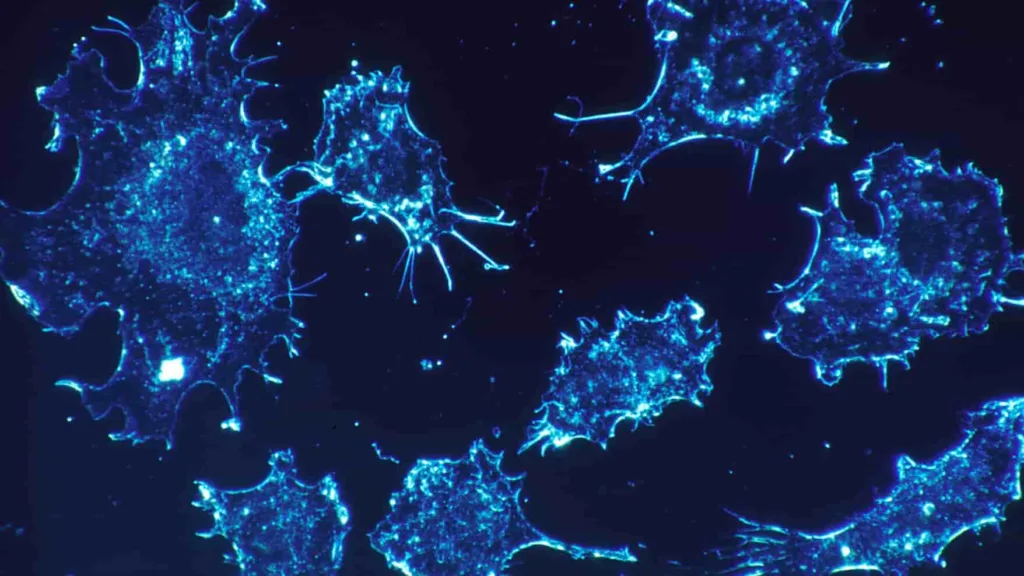
Solid tumours, such as those found in breast and colon cancers, have not, however, shown the same degree of success.
Since solid tumours are composed of a mixture of cells with different antigens, many of which may be the same as those on healthy cells, they present a more complicated picture. Because of this, identifying a solid target for CAR-T cell therapy has proven extremely difficult, with many early initiatives coming to a standstill.
A Groundbreaking Cancer Fighting Method
Associate professor of biomedical engineering Tal Danino has developed a novel strategy to combat these solid tumours with the help of his committed team. Probiotics—also known as “friendly bacteria”—have been cleverly designed to target and penetrate certain tumours. Once there, these bacteria produce artificial signals that help CAR-T cells identify and eradicate the tumour cells by increasing their familiarity.
Danino elaborated on this accomplishment, saying, “CAR-T cells can target a variety of tumour types thanks to our probiotic platform.” “Traditional CAR-T therapies have relied on targeting naturally occurring tumour antigens,” he continued. However, in order to identify synthetic antigens in solid tumours, we are now combining engineered bacteria with designed T cells. There are enormous possible ramifications for cancer treatment.
Danino’s lab has ushered in the era of the “universal” CAR-T cell by utilising this tactic. By instructing the bacteria to label solid tumours with a synthetic identifier, this cell seeks to create a universal marker. As this study advances, it is envisaged that it will become unnecessary to identify a distinct tumour antigen and create a customised CAR-T cell therapy for every type of cancer and patient, greatly simplifying the process.
Advances in Medical Technology
Probiotics direct CAR-T cells on this state-of-the-art ProCAR platform, which is more than just a hybrid of the two. This is the first time that CAR-T cells have responded to artificial antigens made inside the tumour due to a synergistic effect.
Danino’s doctorate student Rosa Vincent, who also served as the study’s co-lead author, offered her thoughts on this novel approach. We envisioned combining the distinctive advantages of two cell therapies, she added. “The T cells then move in to eliminate the harmful cells, with the bacteria acting as the marker.”
Promising Initial Results
Promising outcomes in a range of human and mouse cancer models have been demonstrated by their study. The presence of these modified bacteria within the tumour appeared to favour human T cells in particular, enhancing their capacity to combat cancer cells.
Danino concluded by saying, “Our ProCAR platform offers a revolutionary technique to increase the effects of CAR-T cell treatment on solid tumours.
We are enthusiastic about the potential benefits this could have for cancer treatment, even though we are very early in the study process.
Road Ahead
This ground-breaking research was conducted in tandem with Nicholas Arpaia’s laboratory at Columbia University’s Vagelos College of Physicians and Surgeons, rather than as a stand-alone project. Previously, the two researchers collaborated to create microorganisms that might administer immunotherapy therapies.
Driven by their present discoveries, the scientists are determined to improve their techniques. Their goal is to start clinical studies so they may investigate the efficacy and safety of this platform for treating patients.
These cutting-edge approaches offer millions of cancer patients new hope as science continues to advance and hint at the possibility of more effective and adaptable treatments in the future.
References : http://www.wikipedia.com