Insulin, a hormone produced by the pancreas, is one of the most vital components in the body’s intricate metabolic machinery. This small protein molecule has the essential job of regulating blood sugar levels, allowing the cells to use glucose as fuel. The story of insulin is not just a medical or biological one—it has profoundly changed the lives of millions of people around the world, particularly those with diabetes. From its discovery in the early 20th century to the complex role it plays in managing health today, insulin has been a focal point of modern medicine.
This blog post will take you through everything there is to know about insulin: its functions, the disorders linked to its imbalance, treatments involving insulin, and the future of insulin therapy. By the end, you’ll understand the significance of insulin in human health and disease and why it is so carefully managed in medical treatments.
1. What Is Insulin?
Insulin is a hormone that plays a critical role in glucose metabolism, helping the body maintain homeostasis or balance. It is secreted by the beta cells in the pancreas, specifically in a region known as the Islets of Langerhans. Insulin’s primary function is to lower blood sugar (glucose) levels, ensuring that glucose is transported into cells, where it can be used as an energy source.
Without insulin, cells cannot effectively absorb glucose from the bloodstream, leading to elevated blood sugar levels. If left unchecked, this can cause serious complications, such as damage to organs and tissues. This is especially critical in individuals with diabetes, where insulin production or utilization is impaired.
Chemical Structure
Insulin is a protein composed of 51 amino acids, arranged in two chains (A and B), held together by disulfide bonds. While seemingly small, this molecule is the key to energy regulation across a wide range of biological processes.
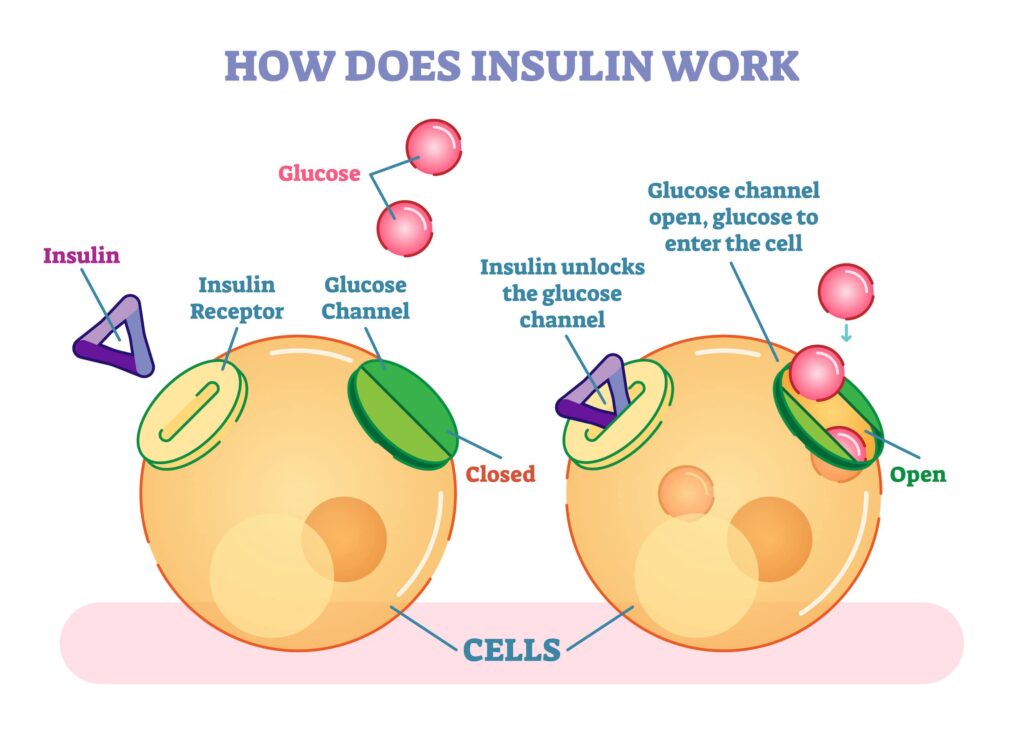
2. How Does Insulin Work in the Body?
After you eat a meal, your digestive system breaks down carbohydrates into glucose, which enters your bloodstream. As blood glucose levels rise, the pancreas responds by releasing insulin into the blood. Insulin then acts like a key, unlocking cells so that they can take up glucose from the bloodstream.
Once inside the cells, glucose is either:
Used immediately as energy, especially in muscle and brain tissues
Stored in the liver as glycogen for later use
Converted into fat if energy needs are low
The Insulin-Glucagon Balance
In addition to insulin, the pancreas also secretes glucagon, another hormone that has the opposite effect of insulin. While insulin lowers blood glucose, glucagon increases it by signaling the liver to release stored glucose when blood sugar levels drop. This balance keeps blood sugar levels stable, ensuring the body has a constant energy supply.
3. The Discovery of Insulin: A Medical Breakthrough
The discovery of insulin in 1921 by Dr. Frederick Banting, Charles Best, and colleagues is one of the most significant milestones in medical history. Before this, being diagnosed with diabetes would mean a death sentence. There was no effective treatment for patients, especially for those with Type 1 diabetes, who often did not live more than a year after diagnosis.
After isolating insulin from the pancreas of animals, Banting and Best successfully tested it on diabetic dogs, and later on human patients. The results were nothing short of miraculous. Within days, patients with severe diabetes, who were on the brink of death, showed remarkable improvement. In 1923, Banting and John Macleod, a colleague, were awarded the Nobel Prize in Medicine for their groundbreaking work.
This discovery revolutionized diabetes treatment and remains a cornerstone of modern medical therapy. Insulin quickly became the first effective treatment for diabetes and saved millions of lives.
4. The Role of Insulin in Diabetes
Diabetes is a disease in which the body either cannot use the insulin it generates efficiently or does not make enough of it. There are several types of diabetes, each with different causes and treatment strategies.
Type 1 Diabetes
In Type 1 diabetes, the body’s immune system mistakenly attacks and destroys the insulin-producing beta cells in the pancreas. As a result, people with Type 1 diabetes cannot produce insulin at all and need to rely on insulin injections or pumps to survive. Type 1 diabetes is typically diagnosed in childhood or adolescence, though it can develop at any age.
Type 2 Diabetes
The most prevalent type of diabetes, known as type 2, is brought on by an increased insulin resistance in the body. This means that insulin is produced, but the body’s cells do not respond to it effectively. Over time, the pancreas cannot keep up with the increased demand for insulin, and blood sugar levels rise. Lifestyle factors such as poor diet, lack of exercise, and obesity are major contributors to the development of Type 2 diabetes.
Gestational Diabetes
Gestational diabetes occurs in some women during pregnancy. Like Type 2 diabetes, it involves insulin resistance, but it usually resolves after childbirth. Nonetheless, Type 2 diabetes is more likely to strike women who have gestational diabetes in the future.
5. Different Types of Insulin and Their Uses
Insulin therapy is essential for individuals with Type 1 diabetes and sometimes necessary for people with Type 2 diabetes. There are different types of insulin, categorized based on how quickly they start working, when they peak, and how long they last.
Rapid-Acting Insulin
Onset: 10-30 minutes after injection
Peak: 30 minutes to 3 hours
Duration: 3-5 hours
Use: Taken before or after meals to control spikes in blood sugar
Short-Acting Insulin
Onset: 30 minutes to 1 hour
Peak: 2-5 hours
Duration: 5-8 hours
Use: Also taken before meals, but its effects last longer than rapid-acting insulin.
Intermediate-Acting Insulin
Onset: 1-2 hours
Peak: 4-12 hours
Duration: 12-18 hours
Use: Usually taken once or twice a day to provide background insulin.
Long-Acting Insulin
Onset: Several hours
Peak: No significant peak
Duration: 24 hours or more
Use: maintains a constant insulin level all day and all night.
6. How Insulin is Administered
For people who require insulin therapy, several delivery methods are available.
Insulin Injections
The most common method is via syringe or insulin pen. Insulin is injected subcutaneously (under the skin) into fatty tissue in areas like the abdomen, thighs, or arms. This method requires multiple daily injections, depending on the type of insulin used.
Insulin Pumps
An insulin pump is a small device worn on the body that delivers a continuous infusion of insulin through a small tube. This method mimics the body’s normal insulin secretion and can be more convenient for those requiring frequent insulin adjustments.
Emerging Technologies
Recent advancements include the development of smart insulin patches, which detect blood sugar levels and deliver insulin accordingly, and the artificial pancreas, which combines continuous glucose monitoring with insulin pumps to automatically adjust insulin delivery.
7. Insulin Resistance and Metabolic Syndrome
Insulin resistance occurs when cells in the muscles, fat, and liver don’t respond well to insulin and can’t use glucose from the blood for energy. To compensate, the pancreas produces more insulin. Over time, this can lead to Type 2 diabetes. Insulin resistance is often associated with metabolic syndrome, a cluster of conditions that increase the risk of heart disease, stroke, and Type 2 diabetes.
Factors Leading to Insulin Resistance
Obesity: Excess body fat, especially around the abdomen, is a key contributor.
Physical Inactivity: Lack of exercise reduces insulin sensitivity.
Poor Diet: Diets high in processed sugars and refined carbohydrates strain the pancreas.
Genetics: Risk is increased by a family history of diabetes.
8. Diet and Lifestyle: Natural Ways to Support Insulin Function
Maintaining a healthy lifestyle can improve insulin sensitivity and lower the risk of developing insulin resistance or Type 2 diabetes.
Exercise Regularly: Physical activity helps muscles use glucose more efficiently.
Eat a Balanced Diet: Focus on whole grains, lean proteins, and plenty of vegetables. Avoid sugary drinks and processed foods.
Maintain a Healthy Weight: Losing even a small percentage of body weight can improve insulin sensitivity.
Get Enough Sleep: Sleep deprivation affects glucose metabolism and increases insulin resistance.
9. The Future of Insulin Therapy
As technology advances, new forms of insulin and delivery methods are on the horizon. One of the most exciting developments is smart insulin, which can automatically adjust its release based on blood sugar levels. Researchers are also exploring gene therapy and stem cell treatments as potential ways to restore natural insulin production in people with Type 1 diabetes.
Additionally, artificial pancreas systems that fully automate blood sugar control are becoming more sophisticated and widely available. These innovations may one day make diabetes management far less burdensome for those who rely on insulin therapy.
10. Frequently Asked Questions
Q1: How do I know if I need insulin therapy?
A: Insulin therapy is typically required for individuals with Type 1 diabetes. For people with Type 2 diabetes, insulin may be prescribed if oral medications and lifestyle changes are not enough to control blood sugar.
Q2: Can insulin cause weight gain?
A: Yes, insulin therapy can lead to weight gain, as it helps the body store glucose for energy. However, maintaining a healthy diet and regular exercise can mitigate this effect.
Q3: Is it possible to manage diabetes without insulin?
A: Some people with Type 2 diabetes can manage their condition with lifestyle changes and oral medications. However, insulin is essential for people with Type 1 diabetes and may become necessary for those with Type 2 diabetes if other treatments are ineffective.
Q4: Can I take insulin if I don’t have diabetes?
A: No, insulin should only be taken under medical supervision for people with diabetes. Using insulin without a prescription can cause dangerously low blood sugar (hypoglycemia).
Q5: What are the side effects of insulin?
A: Common side effects include low blood sugar (hypoglycemia), weight gain, and injection site reactions. Rare but serious side effects can include allergic reactions and insulin resistance over time.
Reference : http://www.mayoclinic.org