Insulin, a hormone produced by the pancreas, plays a crucial role in how our bodies utilize and store energy. It’s the key player in regulating blood sugar levels, facilitating the entry of glucose into cells, and ensuring that the body maintains a delicate balance between energy intake and expenditure. However, when this intricate balance is disturbed—such as in insulin resistance or type 2 diabetes—the body struggles to process glucose efficiently, leading to a host of health complications.
In recent decades, extensive research has emerged showing that exercise is one of the most powerful interventions to improve insulin sensitivity and glucose regulation. Whether you’re looking to prevent metabolic disorders, manage blood sugar, or improve your overall health, understanding the connection between insulin and exercise is essential.
This article explores the complex relationship between insulin and exercise, how different forms of physical activity influence insulin sensitivity, and what this means for overall health.
What Is Insulin? A Quick Overview
Before diving into how exercise impacts insulin, it’s crucial to understand the basic role of insulin in the body. Insulin is a hormone that allows your body to use glucose (sugar) from carbohydrates in the food you eat for energy or to store it for future use. Without insulin, glucose remains in the bloodstream, causing blood sugar levels to rise dangerously high—a condition known as hyperglycemia.
In healthy individuals, the pancreas releases insulin in response to rising blood sugar levels, usually after eating. The hormone binds to receptors on cells, particularly in muscle, liver, and fat tissue, allowing glucose to enter the cells and be utilized for energy. Excess glucose is stored as glycogen in the liver and muscles or converted into fat for long-term energy reserves.
Insulin Resistance: The Silent Disruptor
Insulin resistance is a condition in which the body’s cells become less responsive to the effects of insulin. In other words, more insulin is required to help glucose enter the cells. Over time, insulin resistance can lead to the pancreas producing excessive amounts of insulin in an attempt to normalize blood sugar levels. This eventually exhausts the pancreas and may lead to prediabetes or type 2 diabetes.
Several factors contribute to insulin resistance, including genetics, poor diet, obesity, and a sedentary lifestyle. One of the most well-documented ways to combat insulin resistance is through regular exercise, which enhances the body’s insulin sensitivity.
How Does Exercise Impact Insulin Sensitivity?
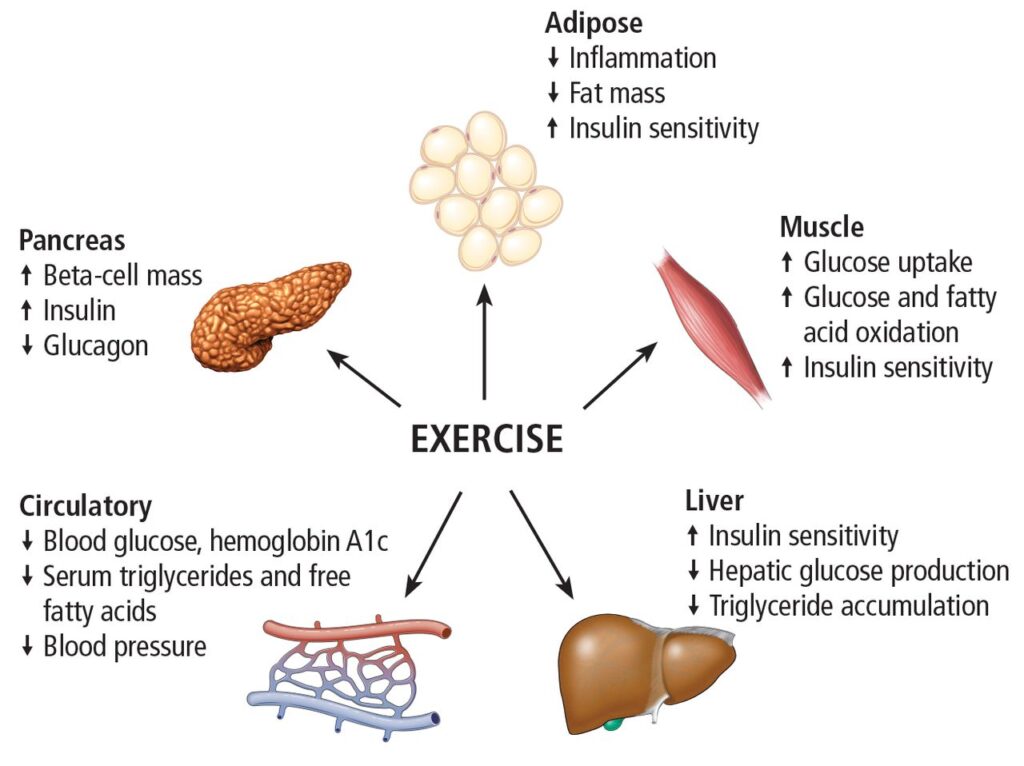
Exercise has profound and immediate effects on insulin sensitivity. When you engage in physical activity, your muscles demand more energy, which means they become more sensitive to insulin to utilize glucose for fuel. This leads to improved glucose uptake and reduced blood sugar levels. Below are some key ways exercise influences insulin:
1. Increased Glucose Uptake
During exercise, muscle cells use more glucose to fuel contractions, particularly in aerobic activities like walking, running, and cycling. As muscle cells use glucose for energy, the body’s sensitivity to insulin increases because it no longer needs high amounts of insulin to bring glucose into the cells.
2. Non-Insulin Mediated Glucose Uptake
Exercise stimulates glucose uptake into cells through non-insulin pathways. This process is mediated by an enzyme known as AMP-activated protein kinase (AMPK), which is activated when energy levels in muscle cells drop during exercise. This mechanism allows glucose to enter cells without needing insulin, providing an alternative route for glucose disposal and enhancing insulin sensitivity.
3. Long-Term Insulin Sensitivity
After exercise, insulin sensitivity remains elevated for 24-48 hours. Regular, consistent exercise causes adaptations in muscle cells, making them more efficient at utilizing glucose and less dependent on insulin. Over time, this reduces the amount of insulin the body needs to maintain stable blood sugar levels.
4. Reduced Inflammatory Markers
Chronic inflammation is a major contributor to insulin resistance. Exercise has anti-inflammatory effects by reducing the levels of pro-inflammatory cytokines and increasing the production of anti-inflammatory molecules like adiponectin. Lowering inflammation helps to improve insulin signaling and prevent insulin resistance.
5. Increased Muscle Mass
Strength training exercises, like weightlifting, have a unique impact on insulin sensitivity. Building more muscle increases the amount of tissue available to absorb glucose from the bloodstream. Since muscle is a highly metabolically active tissue, increasing muscle mass can significantly improve insulin sensitivity.
Exercise Types and How They Affect Insulin Sensitivity
Different forms of exercise can influence insulin sensitivity in unique ways. Here’s a breakdown of how aerobic exercise, resistance training, and high-intensity interval training (HIIT) each play a role:
Aerobic Exercise
Aerobic activities like walking, jogging, swimming, and cycling are highly effective at improving insulin sensitivity, particularly when done regularly. These forms of exercise increase glucose uptake by muscles during and after exercise, lower body fat, and enhance cardiovascular health—all of which contribute to improved insulin function.
Impact on Insulin: Aerobic exercise is linked with improved insulin sensitivity due to increased mitochondrial activity in muscle cells, which helps the body use glucose more efficiently. Even moderate aerobic exercise, such as brisk walking for 30 minutes a day, can significantly improve insulin action.
Resistance Training
Resistance training, such as weightlifting or bodyweight exercises, increases muscle mass and strength, which in turn enhances insulin sensitivity. When you build muscle, you’re essentially creating more space to store glucose. Additionally, resistance training has been shown to improve the muscle’s ability to take up glucose independently of insulin.
Impact on Insulin: Lifting weights has been shown to improve insulin sensitivity by increasing muscle mass and enhancing glucose transport mechanisms within the muscle. It also helps reduce fat mass, which further improves insulin signaling.
High-Intensity Interval Training (HIIT)
HIIT combines short bursts of high-intensity exercise with periods of low-intensity recovery. It’s been gaining popularity for its time efficiency and profound effects on metabolic health, including insulin sensitivity. Studies suggest that HIIT can improve insulin sensitivity more effectively than continuous moderate-intensity exercise, despite requiring less time.
Impact on Insulin: HIIT causes rapid changes in glucose metabolism and enhances insulin sensitivity through increased mitochondrial function and fat oxidation. It also triggers beneficial hormonal responses that further improve insulin action.
The Science Behind Post-Exercise Insulin Sensitivity
After exercising, insulin sensitivity remains heightened for several hours to days, depending on the intensity and duration of the workout. This phenomenon is known as the “afterburn” effect, where muscle cells continue to absorb glucose efficiently, even without high insulin levels.
The mechanism behind this increased sensitivity is multifaceted:
Increased GLUT4 Activity: GLUT4 is a glucose transporter that moves to the surface of muscle cells in response to both insulin and muscle contractions during exercise. After exercise, more GLUT4 transporters remain on the surface, allowing for greater glucose uptake without the need for insulin.
Improved Insulin Signaling: Exercise improves the insulin-signaling cascade, particularly in the muscle cells. This means that the body requires less insulin to achieve the same glucose uptake, which is particularly beneficial for those with insulin resistance or type 2 diabetes.
Exercise and Insulin Resistance: A Preventative and Therapeutic Tool
Exercise is not only preventive but also a therapeutic tool for managing insulin resistance and type 2 diabetes. The American Diabetes Association recommends at least 150 minutes of moderate-intensity aerobic exercise or 75 minutes of vigorous-intensity aerobic exercise per week, combined with two to three sessions of resistance training.
Research shows that both aerobic and resistance exercise are effective in improving insulin sensitivity, with a combination of the two providing the best outcomes. Regular physical activity has been shown to lower A1C levels, a measure of long-term blood glucose control, and reduce the need for diabetes medications.
For individuals at risk of developing diabetes, such as those with prediabetes or metabolic syndrome, exercise can prevent or delay the onset of the disease by improving insulin sensitivity and promoting weight loss.
Exercise Timing and Its Effects on Insulin Sensitivity
When it comes to optimizing insulin sensitivity through exercise, the timing of your workout can make a difference. Exercising in a fasted state, such as first thing in the morning before eating, has been shown to improve insulin sensitivity more effectively than exercising after a meal. This is because the body relies more on stored fat and glycogen when exercising in a fasted state, enhancing the metabolic adaptations that improve insulin action.
Additionally, some studies suggest that exercising after a meal can help lower postprandial blood sugar levels, particularly in individuals with insulin resistance or type 2 diabetes. Post-meal exercise helps the body quickly dispose of glucose from the bloodstream, preventing dangerous spikes in blood sugar.
The Role of Diet and Nutrition in Insulin Sensitivity
While exercise is a powerful tool for improving insulin sensitivity, diet also plays a critical role. A diet rich in whole foods, such as fruits, vegetables, whole grains, lean proteins, and healthy fats, supports insulin function by providing essential nutrients and minimizing the intake of processed, high-sugar foods that can exacerbate insulin resistance.
Combining exercise with a balanced diet can further enhance insulin sensitivity and promote overall metabolic health. Particularly, diets low in refined carbohydrates and sugars, and high in fiber, have been shown to improve blood sugar control and reduce the risk of type 2 diabetes.
Conclusion
The connection between insulin and exercise is a cornerstone of metabolic health. Whether you’re aiming to prevent insulin resistance, manage diabetes, or simply optimize your health, incorporating regular physical activity into your routine is essential. Exercise not only improves insulin sensitivity immediately but also provides long-term benefits by reducing inflammation, increasing muscle mass, and enhancing glucose metabolism. Coupled with a healthy diet, exercise can transform the way your body handles insulin, leading to better blood sugar control and improved overall well-being.
Frequently Asked Questions
Q1: How long does it take for exercise to improve insulin sensitivity?
A1: The effects of exercise on insulin sensitivity can be immediate. After a single session of moderate or high-intensity exercise, insulin sensitivity is elevated for 24-48 hours. However, long-term improvements in insulin sensitivity require consistent exercise over weeks or months.
Q2: Can exercise replace insulin therapy for diabetics?
A2: While exercise can greatly improve insulin sensitivity, it is not a replacement for insulin therapy in people with type 1 diabetes or advanced type 2 diabetes. Exercise should be used in conjunction with medication under the guidance of a healthcare professional.
Q3: Is there an ideal time to exercise for maximizing insulin sensitivity?
A3: Both fasted exercise and post-meal exercise have benefits. Fasted exercise may enhance fat metabolism and insulin sensitivity, while exercising after meals can help lower blood sugar levels. The best time to exercise depends on individual goals and health conditions.
Q4: What types of exercises are best for improving insulin sensitivity?
A4: A combination of aerobic exercises (like walking, running, or cycling) and resistance training (such as weightlifting) is most effective for improving insulin sensitivity. High-intensity interval training (HIIT) is also highly beneficial.
Q5: Can I improve insulin sensitivity with just diet?
A5: Yes, a healthy diet rich in whole foods and low in processed sugars can improve insulin sensitivity. However, the combination of regular exercise and a balanced diet provides the best results.
Reference : http://www.mayoclinic.org