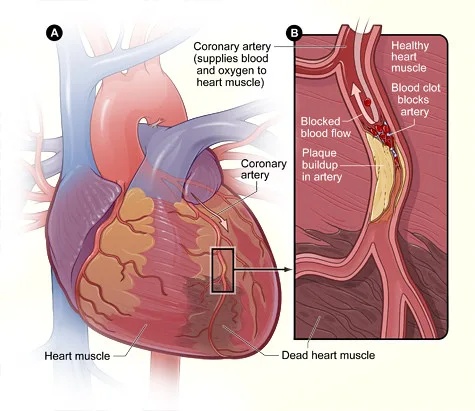
A heart attack, medically known as Myocardial Infarction, occurs when there is a blockage in the blood flow to a part of the heart muscle. This blockage is often caused by a buildup of plaque in the coronary arteries, leading to decreased oxygen supply to the heart tissue. Without adequate oxygen, the affected heart muscle begins to die, resulting in a heart attack.
Differentiating Heart Attack from Cardiac Arrest
It is crucial to differentiate between a heart attack and cardiac arrest as they are two distinct medical emergencies. A heart attack is a circulation problem that occurs when blood flow to the heart is blocked, causing damage to the heart muscle. On the other hand, cardiac arrest is an electrical problem where the heart suddenly stops beating effectively, leading to a cessation of blood flow to the body. While a heart attack can sometimes lead to cardiac arrest, they are not synonymous.
The Role of the Heart and Coronary Arteries
Introduction to the Cardiovascular System
The cardiovascular system is a complex network of organs and vessels responsible for circulating blood throughout the body. At the core of this system lies the heart, a muscular organ that pumps blood to deliver oxygen and nutrients to every cell in the body. Surrounding the heart are the coronary arteries, which supply oxygen-rich blood to the heart muscle itself. Understanding the interplay between the heart and coronary arteries is crucial for comprehending the importance of cardiovascular health.
Anatomy of the Heart
The human heart is roughly the size of a clenched fist and is located slightly left of the center of the chest. It is comprised of four chambers: two atria at the top and two ventricles at the bottom. The atria receive blood returning to the heart, whereas the ventricles circulate blood throughout the body. The heart’s valves ensure that blood flows in the proper direction, avoiding backflow and promoting effective circulation.
Functions of the Heart
The primary function of the heart is to pump blood throughout the body, delivering oxygen and nutrients while removing waste products. This continuous circulation is essential for sustaining life, as every cell depends on a fresh blood supply to function optimally. Additionally, the heart plays a vital role in regulating blood pressure, ensuring that blood flows at an appropriate rate to meet the body’s demands.
Overview of Coronary Arteries
The coronary arteries are a network of blood channels that carry oxygenated blood to the heart muscle. These arteries branch off from the aorta, the body’s main artery, and encircle the heart, providing nourishment to ensure its proper function. Blockages or narrowing of the coronary arteries can lead to serious health conditions, such as coronary artery disease, which can impede blood flow to the heart and result in chest pain or even heart attacks.
Importance of Coronary Artery Health
Maintaining optimal health of the coronary arteries is crucial for overall cardiovascular well-being. Factors such as a healthy diet, regular exercise, and avoidance of smoking can help prevent the buildup of plaque in these vital blood vessels. By promoting good coronary artery health, individuals can reduce their risk of developing heart disease and other cardiovascular complications.
Importance of Early Recognition and Seeking Immediate Medical Attention
Recognizing the symptoms of a heart attack early is paramount as timely intervention can save lives and prevent further damage to the heart. Common symptoms include chest pain or pressure, radiating discomfort to the arm, jaw, or back, shortness of breath, nausea, cold sweats, and lightheadedness. It is crucial to seek immediate medical attention by calling emergency services at the first sign of symptoms.
Causes and Risk Factors of Heart Attacks
Common Causes of Heart Attacks
Atherosclerosis
Atherosclerosis is a condition characterized by the buildup of plaque in the arteries, leading to narrowing and hardening of the blood vessels. This can impede blood flow to the heart, increasing the risk of a heart attack.
High Blood Pressure
Hypertension, or high blood pressure, forces the heart to work harder to pump blood through the body. Over time, this can weaken the heart muscle and increase the likelihood of a heart attack.
High Cholesterol
Elevated levels of cholesterol in the blood can contribute to the formation of plaque in the arteries, further obstructing blood flow to the heart.
Diabetes
Individuals with diabetes are at higher risk of developing heart disease, including heart attacks. Poorly controlled blood sugar levels can damage blood vessels and nerves, increasing the likelihood of cardiovascular complications.
Lifestyle Factors and Heart Attacks
Smoking
Tobacco smoke contains harmful chemicals that can damage blood vessels and increase the risk of blood clots, making smokers more susceptible to heart attacks.
Poor Diet
Diets high in saturated fats, cholesterol, and sodium can contribute to obesity, high blood pressure, and elevated cholesterol levels, all of which are risk factors for heart attacks.
Lack of Physical Activity
Sedentary lifestyles can lead to obesity, high blood pressure, and other risk factors for heart disease. Regular exercise is essential for maintaining cardiovascular health and reducing the risk of heart attacks.
Genetic Predisposition to Heart Attacks
While lifestyle choices play a significant role in determining an individual’s risk of a heart attack, genetic factors also play a role. Family history of heart disease, particularly at a young age, can increase the likelihood of experiencing a heart attack.
Age and Gender as Risk Factors
As individuals age, their risk of developing heart disease, including heart attacks, increases. Men are generally at higher risk of heart attacks than women, although the risk for women rises after menopause.
Medical Conditions and Heart Attacks
Coronary Artery Disease
Coronary artery disease occurs when the coronary arteries that supply blood to the heart become narrowed or blocked by plaque buildup, increasing the risk of a heart attack.
Arrhythmias
Irregular heart rhythms, or arrhythmias, can disrupt the heart’s ability to pump blood effectively, potentially leading to a heart attack.
Heart Failure
Heart failure occurs when the heart is unable to pump enough blood to meet the body’s needs. This can increase the risk of a heart attack due to inadequate blood flow to the heart muscle.
Atherosclerosis:
Atherosclerosis is a condition characterized by the buildup of plaque in the coronary arteries. This plaque consists of cholesterol, fat, calcium, and other substances that can narrow or block the arteries, leading to reduced blood flow to the heart.
Blood Clots Blocking Arteries:
In some cases, a blood clot may form on the surface of a plaque in a coronary artery, further obstructing blood flow. This can trigger a heart attack by cutting off the oxygen supply to a part of the heart muscle.
Other Contributing Factors:
Several factors contribute to the increased risk of a heart attack. These include high blood pressure, high cholesterol levels, smoking, diabetes, obesity, family history of heart disease, advancing age, and certain ethnicities predisposed to heart conditions.
Symptoms of a Heart Attack
Chest Pain or Discomfort
The most commonly reported symptom of a heart attack is chest pain or discomfort. This pain may present as pressure, tightness, or a squeezing sensation in the chest. It can also radiate to the arms, neck, jaw, back, or stomach. The intensity and duration of chest pain can vary from person to person.
Shortness of Breath
Feeling short of breath, especially with minimal exertion or at rest, can be a sign of a heart attack. This symptom may occur with or without chest discomfort and is often accompanied by a rapid or irregular heartbeat.
Nausea and Dizziness
Some individuals experiencing a heart attack may also feel nauseous or lightheaded. These symptoms can be particularly concerning when they occur suddenly and are not attributable to any other underlying condition.
Cold Sweats
Unexplained cold sweats, particularly clammy or profuse sweating, can be indicative of a heart attack. The body’s natural response to stress and pain can manifest as sudden and unprovoked sweating during a heart attack.
Fatigue
Excessive fatigue or sudden onset of weakness, especially in combination with other symptoms like chest pain or shortness of breath, should not be ignored. Fatigue that is out of the ordinary and disrupts daily activities could signal an impending heart attack.
Less Common Symptoms of a Heart Attack
Indigestion or Heartburn
Sometimes, the symptoms of a heart attack can mimic those of indigestion or heartburn. This can lead to delays in seeking medical attention, as the individual may attribute their discomfort to a less serious digestive issue.
Upper Body Pain
In addition to chest pain, a heart attack can cause pain or discomfort in other areas of the upper body, such as the arms (especially the left arm), shoulders, neck, jaw, or upper back. This referred pain is often overlooked or dismissed as muscle soreness.
Unexplained Anxiety
A sense of impending doom or unexplained anxiety can sometimes precede or accompany a heart attack. This feeling of unease may be accompanied by other physical symptoms like chest tightness or shortness of breath.
Recognizing Symptoms in Women
It is important to note that women may experience atypical symptoms during a heart attack compared to men. Women are more likely experience symptoms such as:
Fatigue
Nausea or vomiting
Back or jaw pain
Shortness of breath
Dizziness
These subtle differences underscore the importance of recognizing a diverse range of symptoms when assessing the risk of a heart attack in women.
When to Seek Emergency Help
If you suspect that you or someone else is experiencing a heart attack, it is crucial to act quickly. Do not delay in seeking emergency medical assistance by calling your local emergency number or visiting the nearest hospital. Time is of the essence when it comes to treating a heart attack, and prompt intervention can significantly improve outcomes and reduce complications.
Emergency Response To A Heart Attack
Recognizing the Symptoms
Your first job is to identify the symptoms of a heart attack incase you happen to be in the vicinity of a person having a heart attack. The most common symptoms of heart attack as mentioned above are:
Chest pain or discomfort
Shortness of breath
Nausea or vomiting
Sweating
Pain or discomfort in various parts of the upper body, such as the arms, back, neck, jaw, or stomach
It is important to note that not everyone experiences severe chest pain during a heart attack, especially women and older adults. Any new, unexplained symptoms should not be ignored
Calling for Help
If you suspect that you or someone else is having a heart attack, it is crucial to call emergency services immediately. Time is of the essence in these situations, and quick intervention can make a significant difference in the outcome.
Dial your local emergency number or 911 and provide the dispatcher with all relevant information, including the location, symptoms, and any known medical conditions.
Administering First Aid
While waiting for emergency medical services to arrive, there are several steps you can take to help improve the person’s chances of survival:
Seat down the person or lay him down in a comfortable position.
Loosen any clothing that is tightening the body or putting any pressure and boost the morale of the person by giving assurances that he or she will be alright.
If the person is not allergic to aspirin, have them chew a regular-strength aspirin (325 mg) to help reduce blood clotting.
If the person becomes unconscious and stops breathing normally, start CPR (cardiopulmonary resuscitation) if you are trained to do so.
Providing Ongoing Care
After emergency services have been contacted and first aid measures have been taken, it is important to continue monitoring the person’s condition and providing support:
Stay with the person until help arrives.
Keep them calm and comfortable.
Be prepared to provide information to medical professionals about the onset of symptoms and any actions taken.
Avoid giving the person anything to eat or drink unless instructed by medical personnel.
Preventing Future Heart Attacks
Once the immediate crisis has passed, it is essential to address any underlying risk factors for heart disease to prevent future heart attacks. This may involve lifestyle shifts such as:
Eating a healthy diet rich in vitamins and nutrients avoids saturated fats and cholesterol
Exercising regularly
Maintaining a healthy weight
Managing stress
Quitting smoking
Knowing how to respond effectively in case of a heart attack can save lives. By recognizing the symptoms, calling for help promptly, administering first aid, and providing ongoing care until medical professionals arrive, you can improve the chances of a positive outcome. Remember that time is critical in these situations, so do not hesitate to act if you suspect a heart attack. Stay informed, stay prepared, and stay safe.
Factors Increasing The Risk Of Heart Attack
Age and Gender
Age and gender are key determinants of heart attack risk. Men are generally at a higher risk of heart attacks than premenopausal women. However, the risk for women increases post-menopause, equalizing with that of men. Additionally, the risk of heart attack rises with age, with individuals over 65 facing a significantly higher likelihood compared to younger age groups.
High Blood Pressure
Hypertension, or high blood pressure, is a major risk factor for heart attacks. The increased pressure in the arteries can damage the blood vessels over time, making them more susceptible to blockages. Controlling blood pressure through lifestyle modifications and medication is crucial in reducing the risk of heart attack.
High Cholesterol Levels
Elevated levels of LDL cholesterol, often referred to as “bad” cholesterol, can lead to the buildup of plaque in the arteries, narrowing the passageways through which blood flows. This condition, known as atherosclerosis, increases the risk of heart attack. Maintaining a healthy diet low in saturated fats and cholesterol, along with regular exercise, is essential in managing cholesterol levels.
Smoking and Tobacco Use
Tobacco smoke contains numerous chemicals that can damage blood vessels and increase the formation of arterial plaques. Smokers are at a much higher risk of heart attack compared to non-smokers. Even exposure to secondhand smoke can elevate the risk. Quitting smoking is one of the most effective ways to lower the risk of heart attack.
Diabetes
Individuals with diabetes, especially type 2 diabetes, have a higher risk of heart attack due to elevated blood sugar levels damaging blood vessels over time. Proper management of diabetes through medication, diet, and exercise is essential in reducing the risk of cardiovascular complications, including heart attacks.
Obesity and Physical Inactivity
Being overweight or obese significantly increases the strain on the heart and can lead to conditions such as hypertension, high cholesterol, and diabetes – all of which are major risk factors for heart attacks. In addition, physical inactivity weakens the cardiovascular system, making it more susceptible to cardiac events. Maintaining a healthy weight through a balanced diet and regular exercise is crucial in reducing the risk of heart attack.
Poor Diet
A diet high in unhealthy fats, sugars, and sodium can contribute to various risk factors for heart attack, including obesity, high cholesterol, and hypertension. Consuming a diet rich in fruits, vegetables, whole grains, and lean proteins can help lower the risk of heart attack by promoting overall heart health.
Stress and Mental Health
Chronic stress and poor mental health can have detrimental effects on the cardiovascular system, increasing the risk of heart attack. Stress hormones can elevate blood pressure and contribute to the development of plaque in the arteries. Practicing stress-reducing techniques such as mindfulness, meditation, and regular physical activity can help mitigate this risk factor.
Family History
A family history of heart disease can significantly increase an individual’s risk of experiencing a heart attack. Genetic predispositions combined with shared environmental factors can elevate the likelihood of developing cardiovascular conditions. Understanding your family history and discussing it with your healthcare provider can help tailor preventive strategies to mitigate this risk.
Sleep Apnea
Sleep apnea is a condition characterized by disrupted breathing during sleep, leading to oxygen deprivation and increased stress on the cardiovascular system. Untreated sleep apnea has been linked to an elevated risk of heart attacks. Seeking diagnosis and appropriate treatment for sleep apnea is crucial in reducing this risk factor.
Diagnosis and Treatment of Heart Attacks
Heart health is a critical aspect of overall well-being, and early detection of potential issues can be life-saving. Understanding the tests and diagnostic procedures used to assess heart health is essential for maintaining a healthy heart.
Importance of Heart Health Tests
Regular heart health tests are crucial for early detection of potential issues such as heart disease, high blood pressure, or cholesterol levels. These tests can help in identifying risk factors and implementing preventive measures before a serious condition develops.
Common Heart Health Tests
Electrocardiogram (ECG/EKG)
An ECG is a non-invasive test. ECG test is used to measure the electrical activity of the heart. It helps in detecting abnormal heart rhythms and diagnosing conditions such as arrhythmias or heart attacks.
Echocardiogram
An echocardiogram uses sound waves to create a detailed image of the heart’s structure and function. It helps in assessing the heart’s pumping ability, valves, and chambers.
Stress Test
A stress test involves monitoring the heart’s activity while exercising to evaluate its performance under stress. It helps in diagnosing coronary artery disease and assessing overall cardiovascular fitness.
Cardiac CT Scan
A cardiac CT scan uses advanced imaging technology to visualize the heart’s structure and blood vessels. It is helpful in detecting blockages, aneurysms, or other abnormalities.
Cardiac Catheterization
Cardiac catheterization is an invasive procedure that involves inserting a thin tube into the heart to diagnose and treat various conditions. It helps in measuring blood flow, pressure, and obtaining tissue samples.
Diagnostic Procedures for Heart Health
Blood Tests
Blood tests help in assessing various factors related to heart health, such as cholesterol levels, presence of inflammation, or cardiac enzymes indicating damage to the heart muscle.
Coronary Angiography
Coronary angiography is a procedure that uses contrast dye and X-rays to visualize the coronary arteries. It helps in identifying blockages or narrowing of the arteries.
Holter Monitor
A Holter monitor is a portable device that records the heart’s activity over 24-48 hours. It is useful in detecting irregular heart rhythms that may not be captured during a standard ECG.
Understanding Test Results
After undergoing heart health tests, it is essential to understand the results and their implications. Consultation with a healthcare provider is crucial for interpreting test results accurately and planning further steps if any abnormalities are detected.
Role of Diagnostic Procedures:
Diagnosing a heart attack involves various tests and procedures, including an Electrocardiogram (ECG) to monitor the heart’s electrical activity, blood tests to assess cardiac enzyme levels indicative of muscle damage, echocardiogram for imaging the heart’s structure and function, and angiography to visualize blockages in coronary arteries.
Treatment Options:
Medications for Heart Attacks:
Once a heart attack is suspected or diagnosed, several medications may be administered to help stabilize the patient and improve blood flow to the heart. These medications may include:
Aspirin: to reduce blood clotting and prevent further blockages.
Thrombolytics: to dissolve blood clots and restore blood flow to the heart.
Beta-blockers: for workload reduction on the heart and to lower blood pressure.
ACE inhibitors: to improve heart function and prevent future complications.
Statins: to lower cholesterol levels and reduce the risk of future heart attacks.
Cardiac Procedures for Heart Attacks:
In addition to medications, several cardiac procedures may be performed to treat a heart attack and restore blood flow to the heart. These procedures include:
Angioplasty and stenting: a minimally invasive procedure to open blocked arteries and insert a stent to keep the artery open.
Coronary artery bypass grafting (CABG): a surgical procedure to bypass blocked arteries using blood vessels from other parts of the body.
Thrombectomy: a procedure to remove blood clots from the coronary arteries.
Atherectomy: a procedure to remove plaque buildup from the arteries using a special catheter.
Emotional Support and Rehabilitation:
Recovering from a heart attack can be emotionally challenging, and many individuals may experience anxiety, depression, or post-traumatic stress disorder. Seeking emotional support from healthcare providers, counselors, or support groups can help individuals cope with these feelings and improve their overall well-being. Cardiac rehabilitation programs can also provide education, exercise training, and emotional support to help individuals recover from a heart attack and prevent future cardiac events.
Rehabilitation and Lifestyle Changes:
Following a heart attack, patients are often advised to participate in cardiac rehabilitation programs aimed at physical activity guidance, dietary modifications, stress management techniques, and smoking cessation support. Adopting these lifestyle changes can improve heart health and reduce the risk of future cardiac events.
Prevention Strategies for Heart Attacks
Managing Risk Factors:
Effective prevention of heart attacks entails managing underlying risk factors such as hypertension, hypercholesterolemia, diabetes, obesity, and smoking. Regular monitoring of these conditions and adherence to prescribed medications are essential preventive measures.
Healthy Lifestyle Choices:
Encouraging healthy lifestyle habits like following a balanced diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats; engaging in regular physical activity; maintaining a healthy weight; managing stress levels; and quitting smoking can significantly reduce the risk of developing cardiovascular diseases.
Resources for Lifestyle Guidance:
Educational resources such as nutrition counseling services, exercise programs tailored for cardiovascular health, stress reduction workshops, smoking cessation support groups, and community wellness initiatives can provide individuals with the tools necessary for adopting and sustaining healthy lifestyle choices.
Living with Heart Attack
Emotional and Psychological Impact:
Experiencing a heart attack can have profound emotional and psychological effects on individuals. Fear, anxiety about recurrence, depression due to lifestyle changes, and adjustment to medication regimens are common challenges faced post-heart attack. Seeking support from mental health professionals or joining support groups can aid in coping with these emotional stressors.
Adherence to Medications and Lifestyle Changes:
To prevent future cardiac events and promote overall well-being post-heart attack, it is crucial for individuals to adhere diligently to prescribed medications such as antiplatelets, statins, beta-blockers, and lifestyle modifications recommended by healthcare providers. Consistency in medication intake and lifestyle adjustments significantly contribute to long-term cardiovascular health.
Advancements in Heart Attack Treatment and Research:
In recent years, significant advancements in the treatment and research of heart attacks have revolutionized the way healthcare professionals approach this life-threatening condition. From innovative technologies to groundbreaking research, the landscape of heart attack care is constantly evolving. This blog post delves into the latest developments in heart attack treatment and research, shedding light on the cutting-edge approaches that are shaping the future of cardiovascular healthcare.
Traditional Treatments for Heart Attacks
Historically, the standard treatments for heart attacks have included medications such as antiplatelet agents, beta-blockers, and statins to manage symptoms and reduce the risk of further cardiac events. In cases of severe blockages, procedures like angioplasty and stent placement may be performed to restore blood flow to the heart. While these interventions have been effective in saving lives, there is a constant need for innovation to improve outcomes and patient care.
Advancements in Imaging Technologies
One area where significant progress has been made is in imaging technologies for the diagnosis and treatment of heart attacks. Advanced imaging modalities such as cardiac MRI and CT angiography allow healthcare providers to visualize the heart in unprecedented detail, helping to identify blockages, assess cardiac function, and guide treatment decisions. These non-invasive techniques enable more precise and personalized care for patients with heart attacks.
Novel Therapies and Interventions
In recent years, researchers have been exploring novel therapies and interventions aimed at improving outcomes for patients with heart attacks. One promising approach is the use of stem cell therapy to regenerate damaged heart tissue and promote cardiac repair. Clinical trials are also underway to investigate the potential benefits of gene therapy, tissue engineering, and other cutting-edge treatments for heart attack patients.
Precision Medicine in Cardiology
The concept of precision medicine, which involves tailoring medical treatment to individual characteristics such as genetics, lifestyle, and environment, is gaining traction in cardiology. By leveraging advances in genomics and molecular diagnostics, healthcare providers can identify patients at higher risk of heart attacks and customize treatment plans to optimize outcomes. Precision medicine holds great promise for improving the effectiveness and safety of heart attack care.
Lifestyle Interventions and Preventive Strategies
In addition to medical therapies and interventions, lifestyle modifications play a crucial role in preventing heart attacks and reducing cardiovascular risk. Encouraging patients to adopt healthy habits such as regular exercise, a balanced diet, smoking cessation, and stress management can significantly impact their heart health. Healthcare providers are increasingly emphasizing the importance of holistic approaches to cardiovascular care that address both medical and lifestyle factors.
Collaborative Care Models
Another trend in the management of heart attacks is the shift towards collaborative care models that involve multidisciplinary teams of healthcare professionals working together to provide comprehensive and coordinated care. This approach ensures that patients receive timely interventions, follow-up care, and support services from a diverse group of experts, including cardiologists, nurses, dietitians, and physical therapists. By fostering teamwork and communication, collaborative care models enhance patient outcomes and satisfaction.
Patient Education and Empowerment
Empowering patients with knowledge about heart attacks, risk factors, and self-care strategies is essential for improving outcomes and reducing recurrence rates. Education programs that focus on medication adherence, symptom recognition, lifestyle modifications, and emergency response can help patients take an active role in managing their heart health. By promoting awareness and self-advocacy, healthcare providers can empower individuals to make informed decisions about their treatment and recovery journey.
Future Directions in Heart Attack Research
Looking ahead, the future of heart attack research holds exciting possibilities for advancing our understanding of cardiovascular disease and developing innovative therapies. Emerging areas of interest include artificial intelligence for predictive analytics, wearable devices for remote monitoring, and nanotechnology for targeted drug delivery. By embracing technological advancements and interdisciplinary collaboration, researchers are poised to make further strides in the prevention, diagnosis, and treatment of heart attacks.
To sum it up, the field of heart attack treatment and research is experiencing rapid evolution driven by scientific discovery, technological innovation, and a patient-centered approach to care. From personalized medicine to lifestyle interventions to collaborative care models, the landscape of cardiovascular healthcare is being transformed to better meet the needs of patients with heart attacks. By staying informed about the latest advancements and advocating for comprehensive solutions, we can collectively contribute to a future where heart attacks are not only treatable but preventable.
Ongoing research efforts continue to explore innovative treatment modalities for heart attacks such as stem cell therapy, gene-based therapies, and personalized medicine approaches tailored to individual patient profiles. These advancements hold promise for improving outcomes and enhancing recovery post-heart attack.
Role of Technology in Prevention and Management:
Technological innovations like wearable devices for continuous monitoring of vital signs, telemedicine platforms for remote consultations with healthcare providers, mobile applications for tracking diet and exercise routines, and artificial intelligence algorithms for risk prediction play a vital role in preventing heart attacks and managing cardiovascular health effectively.
Addressing Disparities in Heart Attack Risk and Access to Care:
Disparities in heart attack risk factors exist among different demographic groups due to socioeconomic factors, geographical location, cultural beliefs, and healthcare access limitations. Initiatives focusing on health equity through community outreach programs, culturally competent care delivery models, and policy advocacy aim to bridge these gaps and ensure equitable access to preventive services and quality care for all individuals.
Myths and Misconceptions About Heart Attacks
Heart attacks are the single most common cause of death globally. Despite the high prevalence of this condition, there are numerous myths and misconceptions surrounding heart attacks that can lead to confusion and misinformation. Let us debunk some of the most common myths and misconceptions about heart attacks and provide accurate information to help you better understand this life-threatening condition.
Myth – Only older individuals are at risk of heart attacks
One of the most common myths about heart attacks is that they only affect older individuals. While it is true that the risk of heart attacks increases with age, young and middle-aged individuals are also susceptible to this condition. Several factors, such as family history, smoking, high cholesterol, high blood pressure, diabetes, and obesity, can increase the risk of heart attacks in individuals of all ages.
Myth – Heart attacks always cause chest pain
Another prevalent myth about heart attacks is that they always present with severe chest pain. While chest pain is a common symptom of a heart attack, not all individuals experience this symptom. Some people may have atypical symptoms such as shortness of breath, nausea, lightheadedness, or pain in other parts of the body, such as the jaw, neck, back, or arms. It is essential to be aware of these diverse symptoms to seek prompt medical attention in case of a heart attack.
Myth – Women are not as likely to have heart attacks as men
There is a misconception that heart attacks predominantly affect men and that women are less likely to experience this condition. In reality, heart disease is the most common cause of death for women in the United States. However, women may present with different symptoms than men and are often underdiagnosed and undertreated for heart attacks. It is crucial for both men and women to be aware of the risk factors and symptoms of heart attacks to receive timely medical intervention.
Myth – If you have a healthy lifestyle, you are immune to heart attacks
While maintaining a healthy lifestyle can significantly reduce the risk of heart attacks, it does not guarantee immunity against this condition. Genetic factors, underlying medical conditions, and environmental factors can also contribute to the development of heart attacks. It is essential to combine a healthy diet, regular exercise, stress management, and routine medical check-ups to minimize the risk of heart attacks effectively.
Myth – Heart attacks are always fatal
Contrary to popular belief, not all heart attacks are fatal. With advancements in medical technology and prompt intervention, many individuals survive heart attacks and go on to lead healthy lives. The key to improving the outcomes of a heart attack is recognizing the symptoms early, seeking immediate medical attention, and following a comprehensive treatment plan prescribed by healthcare professionals. Early intervention can save lives and prevent long-term complications associated with heart attacks.
Myth – Heart attacks only occur in individuals with pre-existing heart conditions
While individuals with pre-existing heart conditions are at a higher risk of heart attacks, anyone can experience this medical emergency. Factors such as smoking, poor dietary habits, sedentary lifestyle, obesity, high stress levels, and underlying health conditions like diabetes and hypertension can increase the likelihood of a heart attack in otherwise healthy individuals. It is crucial to adopt a proactive approach to heart health through preventive measures and regular screenings to detect any potential risk factors early.
Myth – You can self-diagnose and treat a heart attack at home
One dangerous myth about heart attacks is the belief that individuals can self-diagnose and treat a heart attack at home. This misconception can lead to delays in seeking appropriate medical care, which can be life-threatening during a heart attack. If you suspect that you or someone else is experiencing symptoms of a heart attack, such as chest discomfort, shortness of breath, nausea, or lightheadedness, it is imperative to call emergency services immediately. Only trained healthcare professionals can accurately diagnose a heart attack and initiate timely treatment to improve outcomes.
Myth – Aspirin is a cure for a heart attack
There is a common misconception that taking aspirin during a heart attack can cure the condition or alleviate symptoms. While aspirin can help reduce blood clotting and improve blood flow during a heart attack, it is not a definitive cure for the underlying issue. Aspirin should only be taken under the guidance of healthcare providers during a suspected heart attack or as part of a long-term treatment plan for individuals at high risk of cardiovascular events. It is essential to follow medical advice and treatment protocols tailored to each individual’s specific health needs.
Myth – Once the symptoms of a heart attack subside, there is no need for medical attention
Some individuals may experience temporary relief from the symptoms of a heart attack and assume that the episode has passed without the need for medical intervention. However, it is crucial to understand that not all heart attacks present with persistent symptoms. Silent heart attacks, which occur without noticeable symptoms, can still cause significant damage to the heart muscle and increase the risk of future cardiovascular events. Any suspicion of a heart attack should prompt an immediate evaluation by healthcare professionals to assess the extent of damage and implement appropriate treatment strategies.
Debunking Myths Leads to Better Heart Health
Debunking myths and misconceptions about heart attacks is essential for promoting awareness, early detection, healthy heart and effective management of this life-threatening condition. By understanding the facts surrounding heart attacks and dispelling common myths, individuals can take proactive steps towards improving their heart health and reducing the risk of cardiovascular events. It is crucial to stay informed, prioritize preventive care, and seek prompt medical attention in case of any concerning symptoms related to heart health.
By following the recommendations outlined in this comprehensive guide to heart health tests and diagnosis, you can take proactive steps towards maintaining a healthy heart and overall well-being. Remember that early detection and preventive measures play a crucial role in promoting heart health and reducing the risk of cardiovascular diseases. Stay informed, stay proactive, and prioritize your heart health for a healthier future.
Frequently Asked Questions (FAQs)
1. Can stress trigger a heart attack? Stress can contribute to an increased risk of heart attacks by elevating blood pressure and releasing stress hormones that can strain the cardiovascular system over time. Managing stress through relaxation techniques, exercise, and counseling can help reduce the risk of heart attacks.
2. What role does family history play in heart attacks? A family history of heart disease can predispose individuals to an increased risk of heart attacks due to genetic factors that influence cholesterol levels, blood pressure regulation, and overall cardiovascular health. Knowing your family history can help healthcare providers assess your risk and tailor preventive strategies accordingly.
3. Are all heart attacks the same? Not all heart attacks are identical. The type and severity of a heart attack can vary based on factors such as the location of blockages in the coronary arteries, the extent of damage to the heart muscle, and individual risk factors. Healthcare professionals use diagnostic tests to classify heart attacks and develop personalized treatment plans for each patient.
4. How can I prevent a heart attack? Preventing a heart attack involves adopting a healthy lifestyle that includes regular exercise, a balanced diet rich in fruits and vegetables, maintaining a healthy weight, quitting smoking, managing stress effectively, monitoring blood pressure and cholesterol levels regularly, and adhering to prescribed medications as directed by healthcare providers.
5. What should I do if I suspect someone is having a heart attack? If you suspect someone is having a heart attack, call emergency services immediately and provide basic life support measures such as assisting with prescribed medications (e.g., aspirin), ensuring a clear airway, monitoring vital signs, and staying with the individual until help arrives. Prompt action can make a significant difference in the outcome of a heart attack.
6: How often should I undergo heart health tests?
A: The frequency of heart health tests depends on individual risk factors and medical history. Consult your healthcare provider to determine an appropriate testing schedule.
7: Are heart health tests covered by insurance?
A: Many heart health tests are covered by insurance, especially if they are deemed medically necessary. you must confirm with your insurance provider for exact coverage details.
8: What should I do if my test results show abnormalities?
A: If your test results indicate abnormalities, follow up with your healthcare provider for further evaluation and treatment options. It is important not to ignore any concerning findings.
9: Can lifestyle changes improve heart health without medication?
A: Yes, adopting healthy lifestyle habits such as regular exercise, a balanced diet, and stress management can significantly improve heart health and reduce the risk of developing cardiovascular conditions.
10: Are there any specific risk factors that increase the likelihood of heart issues?
A: Risk factors such as high blood pressure, high cholesterol, diabetes, obesity, smoking, and a sedentary lifestyle can significantly increase the risk of heart-related problems. It is important to address these risk factors through lifestyle modifications and medical interventions.
Disclaimer : This article is for informational purposes only, any action should be taken only after consulting the medical practitioner only.
Reference : http://www.webmd.com